top of page
Postpartum Matters
Search


From Hopelessness to Well-Being: Finding Meaning in Hard Times
Karen Kleiman, Owner, The Postpartum Stress Center, The Karen Kleiman Training Center, and author of Good Moms Have Scary Thoughts and...
kkleiman
Dec 22, 2024


The Incubator: Random thoughts of a premature paradox
Reposting old post on behalf of PREMATURITY DAY I wonder, now, why I have such conflicting thoughts about this place. A place I knew as...
kkleiman
Nov 17, 2024


Tragedy & Joy: A Painful Oxymoron
My clients are suffering from all of the suffering. There's so much pain, all around. It's everywhere. I know it and feel it. They know...
kkleiman
Oct 10, 2024


Tips for Talking to Your Provider
Choose the healthcare provider you are most comfortable with, whether it’s your obstetrician, pediatrician, midwife, or family doctor....
kkleiman
Aug 14, 2024


Postpartum Depression: Whose Problem is it?
Healthcare providers please take heed. Postpartum depression and anxiety are getting tons of attention in the media. From catastrophic...
kkleiman
Aug 5, 2024


A Note to New Dads - You might think you're just irritable but you could be depressed.
You might not want to hear this, but if you're not feeling so good since having a baby, it's possible that you may be experiencing...
kkleiman
May 21, 2024


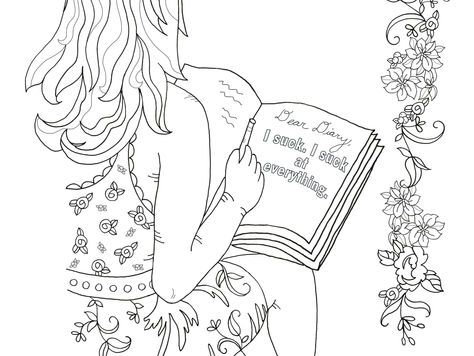
9 Ways Motherhood Can Break Your Spirit (& tips to help you heal)
Source: 123rf.com Postpartum depression and anxiety are getting more attention now than ever before. That's the good news. The...
kkleiman
May 13, 2024


ASK FOR HELP: It can be a matter of life and death
I don’t have a problem asking for help. That’s partly because I don’t pretend to be strong and independent if I’m not feeling that way at...
kkleiman
Mar 17, 2024

What You Didn't Expect When You Were Expecting
20 years ago...... Karen Kleiman was talking about protecting new moms from the pitfalls of unrealistic expectations and how transparency...
kkleiman
Dec 18, 2023


Do Not Stop Until You Find the Right Help
This is what you should do if you think you might have postpartum depression You've recently had a baby. You are more than 3 weeks...
kkleiman
Nov 21, 2023
bottom of page



